Medicines containing nomegestrol or chlormadinone: PRAC recommends new measures to minimise risk of meningioma
EMA’s safety committee (PRAC) has recommended new measures to minimise the risk of meningioma with medicines containing nomegestrol or chlormadinone, which are used for gynaecological and menstrual disorders, hormone replacement therapy and, at lower doses, as hormonal contraceptives (birth control).
Meningioma is a tumour of the membranes covering the brain and spinal cord. It is usually benign and is not considered to be a cancer, but due to their location in and around the brain and spinal cord, meningiomas can in rare cases cause serious problems.
The PRAC has recommended that medicines containing high-dose chlormadinone (5-10 mg) or high-dose nomegestrol (3.75 – 5 mg) should be used at the lowest effective dose and for the shortest duration possible, and only when other interventions are not appropriate. In addition, low- and high-dose nomegestrol or chlormadinone medicines must not be used by patients who have, or have had, meningioma.
As well as restricting the use of the high-dose medicines, the PRAC has recommended that patients should be monitored for symptoms of meningioma. If a patient is diagnosed with meningioma, treatment with these medicines must be permanently stopped.
More information is available in EMA’s public health communication.
PRAC starts review on risk of neurodevelopmental disorders with topiramate
PRAC has started a review of topiramate to assess new data on a potential risk of neurodevelopmental disorders in children who have been exposed to the medicine during pregnancy.
Topiramate is indicated for the treatment of epilepsy, either used alone (monotherapy) or in conjunction with other medicines (combination therapy), as well as for the prevention of migraine. The use of topiramate by pregnant women is already known to increase the risk of birth defects. For that reason, women with epilepsy are advised to avoid becoming pregnant whilst being treated with topiramate, and to consult their doctor for advice in case they wish to become pregnant. Pregnant women, or women of childbearing potential not using highly effective birth control, must not be treated for prevention of migraine.
Recently, a study1 investigating the risk of neurodevelopmental disorders, including autism spectrum disorder and intellectual disability, associated with several anti-epileptic drugs, including topiramate, has been published. The study is based on Nordic registry data and includes more than 24,000 children exposed in utero to at least one anti-epileptic drug, including 471 who were exposed to topiramate.
The study conclusions suggest a possible increase in the risk of autism spectrum disorders, intellectual disability and child neurodevelopmental disorders with the exposure to topiramate during pregnancy.
In light of the importance of this new information, the PRAC decided that further assessment is warranted to determine the scope and the best regulatory procedure to assess these potential risks.
Data from the study is being assessed as a ’safety signal’ - information on new or changes in known adverse events that may potentially be associated with a medicine and that warrants further investigation.
EMA will communicate further as soon as more information becomes available.
New safety information for healthcare professionals
As part of its advice on safety-related aspects to other EMA committees, the PRAC discussed a direct healthcare professional communication (DHPC) containing important information for medicines containing chlormadinone or nomegestrol.
Medicines containing nomegestrol or chlormadinone: new measures to minimise the risk of meningioma
This DHPC aims to inform healthcare professionals that medicines containing high doses of chlormadinone or nomegestrol should only be indicated when other interventions are considered inappropriate. Furthermore, all medicines containing nomegestrol or chlormadinone must not be used by patients who have, or have had, meningioma. Further advice to healthcare professionals in line with the outcome of the PRAC review is also given.
The DHPC will be forwarded to EMA’s human medicines committee (CHMP). Following the CHMP decision, the DHPC will be disseminated to healthcare professionals by the marketing authorisation holder, according to an agreed communication plan, and published on the Direct healthcare professional communications page and in national registers in EU Member States.
PRAC celebrates its tenth anniversary
The July plenary has marked the tenth anniversary of the PRAC, which held its first meeting in July 2012. Since its establishment, the PRAC has held a total of 112 plenary meetings in which more than 3,900 safety topics have been discussed, highlighting the committee’s central role in safeguarding the safety of medicines in the European Union (EU).
1Bjørk M, Zoega H, Leinonen MK, et al. Association of Prenatal Exposure to Antiseizure Medication With Risk of Autism and Intellectual Disability. JAMA Neurol. Published online May 31, 2022. doi:10.1001/jamaneurol.2022.1269.
Agenda
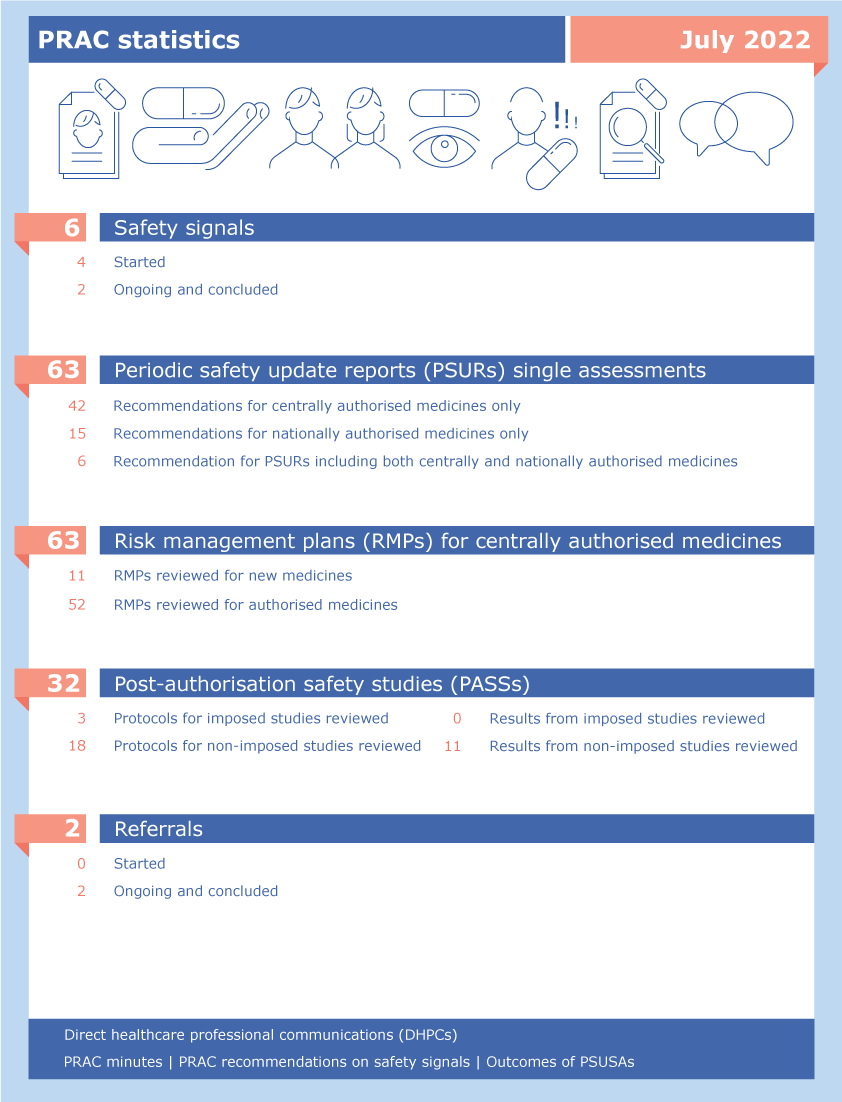
PRAC statistics: July 2022
Glossary:
- Safety signal assessments. A safety signal is information which suggests a new potentially causal association, or a new aspect of a known association between a medicine and an adverse event that warrants further investigation. Safety signals are generated from several sources such as spontaneous reports, clinical studies and the scientific literature. More information can be found under 'Signal management'.
- Periodic safety update reports, abbreviated as PSURs, are reports prepared by the marketing authorisation holder to describe the worldwide safety experience with a medicine in a defined period after its authorisation. PSURs for medicinal products that contain the same active substance or the same combination of active substances but have different marketing authorisations and are authorised in different EU Member States, are jointly assessed in a single assessment procedure. More information can be found under 'Periodic safety update reports: questions and answers'.
- Risk management plans, abbreviated as RMPs, are detailed descriptions of the activities and interventions designed to identify, characterise, prevent or minimise risks relating to medicines. Companies are required to submit an RMP to EMA when applying for a marketing authorisation. RMPs are continually updated throughout the lifetime of the medicine as new information becomes available. More information is available under 'Risk-management plans'.
- Post-authorisation safety studies, abbreviated as PASSs, are studies carried out after a medicine has been authorised to obtain further information on its safety, or to measure the effectiveness of risk-management measures. The PRAC assesses the protocols (aspects related to the organisation of a study) and the results of PASSs. More information can be found under 'Post-authorisation safety studies'.
- Referrals are procedures used to resolve issues such as concerns over the safety or benefit-risk balance of a medicine or a class of medicines. In a referral related to safety of medicines, the PRAC is requested by a Member State or the European Commission to conduct a scientific assessment of a particular medicine or class of medicines on behalf of the EU. More information can be found under referral procedures.
- Summary safety reports have been introduced as part of the enhanced safety monitoring of COVID-19 vaccines. Marketing authorisation holders are required to submit these reports to EMA, starting on a monthly basis. Their submission complements the submission of PSURs. For more information see Pharmacovigilance plan of the EU Regulatory Network for COVID-19 vaccines.
Ongoing referrals
Procedure | Status | Update |
|---|---|---|
| Janus Kinase inhibitors (JAKi) – Article 20 Referral | Under evaluation | PRAC continued its assessment |
| Nomegestrol and chlormadinone - Article - 31 Referral | Under evaluation | PRAC continued its assessment |