New measures for terlipressin-containing medicines in the treatment of hepatorenal syndrome
EMA’s safety committee (PRAC) recommended new measures to reduce the risk of respiratory failure (severe breathing difficulties that may be life-threatening) and sepsis (when bacteria and their toxins circulate in the blood, leading to organ damage) when using terlipressin-containing medicines in people with type 1 hepatorenal syndrome (HRS-1) (kidney problems in people with advanced liver disease).
Terlipressin is a vasopressin analogue. This means that it works in a similar way as the natural hormone vasopressin to cause narrowing of certain blood vessels in the body, in particular those that supply the abdominal organs. In patients with HRS-1, increased blood pressure in the liver due to liver failure leads to widening of these blood vessels, resulting in poor blood supply to the kidneys. By narrowing the blood vessels that supply the abdominal organs, terlipressin helps to restore blood flow to the kidneys, thereby improving kidney function.
The new measures include adding to the product information a warning to avoid terlipressin-containing medicines in patients with advanced acute-on-chronic liver disease (liver disease that suddenly worsens) or advanced kidney failure. Patients with breathing problems should receive treatment to manage their condition before starting terlipressin. During and after treatment, patients should be monitored for signs and symptoms of respiratory failure and infection.
The recommendations follow the PRAC’s review of available data, including results from a clinical trial1 involving patients with HRS-1 which suggested that patients who were treated with terlipressin-containing medicines were more likely to experience and die from respiratory disorders within 90 days after the first dose than those who were given placebo (a dummy treatment).
The recommendations are described further in the section below “New safety information for healthcare professionals”.
More information is available in EMA’s public health communication.
Codeine with ibuprofen: PRAC adds warning for serious renal and gastrointestinal harms
The PRAC has recommended a change to the product information for codeine with ibuprofen combination medicines to include a warning of serious harms, including death, particularly when taken for prolonged periods at higher than recommended doses.
Codeine with ibuprofen is a combination of two medicines, an opioid (codeine) and an anti-inflammatory (ibuprofen), which are used to treat pain. Repeated use of codeine with ibuprofen may lead to dependence (addiction) and abuse due to the codeine component.
The committee reviewed several cases of renal, gastrointestinal and metabolic toxicities that have been reported in association with cases of abuse of and dependence from codeine with ibuprofen combinations, some of which have been fatal.
The PRAC found that, when taken at higher than recommended doses or for a prolonged period of time, codeine with ibuprofen can cause damage to the kidneys, preventing them from removing acids properly from the blood into the urine (renal tubular acidosis). Kidney malfunction can also cause very low levels of potassium in the blood (hypokalaemia), which in turn may cause symptoms such as muscle weakness and light-headedness. Therefore, renal tubular acidosis and hypokalaemia will be added to the product information as new side effects.
As medicines containing a combination of codeine and ibuprofen are authorised at national level, the PRAC has agreed key messages that national competent authorities can use when drafting their communication to relevant healthcare professionals and to inform patients of signs of abuse and dependence, and risks of serious harm. Patients should be advised to consult their doctor if they want to use codeine with ibuprofen for longer than recommended and/or at higher-than-recommended doses.
The PRAC also noted that there are medicines containing codeine with ibuprofen which are available without medical prescription in the EU. As most of these cases were reported in countries where these medicines are available without a prescription, the PRAC considered that prescription-only medicine status would be the most effective risk minimisation measure to mitigate the harm associated with abuse and dependence of these products.
PRAC’s recommendations, together with key messages for communication will be sent to the national competent authorities who can decide on the need for additional communication at national level.
New safety information for healthcare professionals
As part of its advice on safety-related aspects to other EMA committees, the PRAC discussed direct healthcare professional communications (DHPCs) containing important information for terlipressin-containing medicines and Imbruvica.
Terlipressin: new recommendations for patients with type 1 hepatorenal syndrome
This DHPC is intended to inform healthcare professionals of an increased risk of respiratory failure and sepsis or septic shock in patients with type 1 hepatorenal syndrome (type 1 HRS) with terlipressin-containing medicines. This recommendation by the PRAC follows the review of available data, including results from a large clinical trial.
Imbruvica (ibrutinib): new risk minimisation measures, including dose modifications, due to the increased risk for serious cardiac events
This DHPC aims to inform healthcare professionals about an increased risk of fatal and serious cardiac arrhythmias and cardiac failure with the use of ibrutinib.
Imbruvica is a medicine for treating the blood cancers mantle cell lymphoma, chronic lymphocytic leukaemia (CLL) and Waldenström’s macroglobulinaemia (also known as lymphoplasmacytic lymphoma).
Patients with advanced age, Eastern Cooperative Oncology Group (ECOG) performance status ?2, or cardiac co-morbidities may be at greater risk of cardiac events including sudden fatal cardiac events.
The PRAC advises that a clinical evaluation of cardiac history and function should be performed before starting a treatment with ibrutinib. In patients with risk factors for cardiac events, benefits and risks should be assessed before initiating treatment with the medicine and alternative treatment may be considered. Patients should be carefully monitored during treatment for signs of deterioration of cardiac function and be clinically managed.
Ibrutinib should be withheld for any new onset or worsening of grade 2 cardiac failure or grade 3 cardiac arrhythmias. Treatment may be resumed as per new dose modification recommendations.
The DHPC for Imbruvica will be forwarded to EMA’s human medicines committee (CHMP). Following the CHMP decision, the DHPC will be disseminated to healthcare professionals by the marketing authorisation holder, according to an agreed communication plan, and published on the ‘Direct healthcare professional communications’ page and in national registers in EU Member States.
1 Wong F, et al. Terlipressin plus albumin for the treatment of type 1 hepatorenal syndrome. N Engl J Med. 2021 Mar 4;384(9):818-828. doi: 10.1056/NEJMoa2008290
Agenda
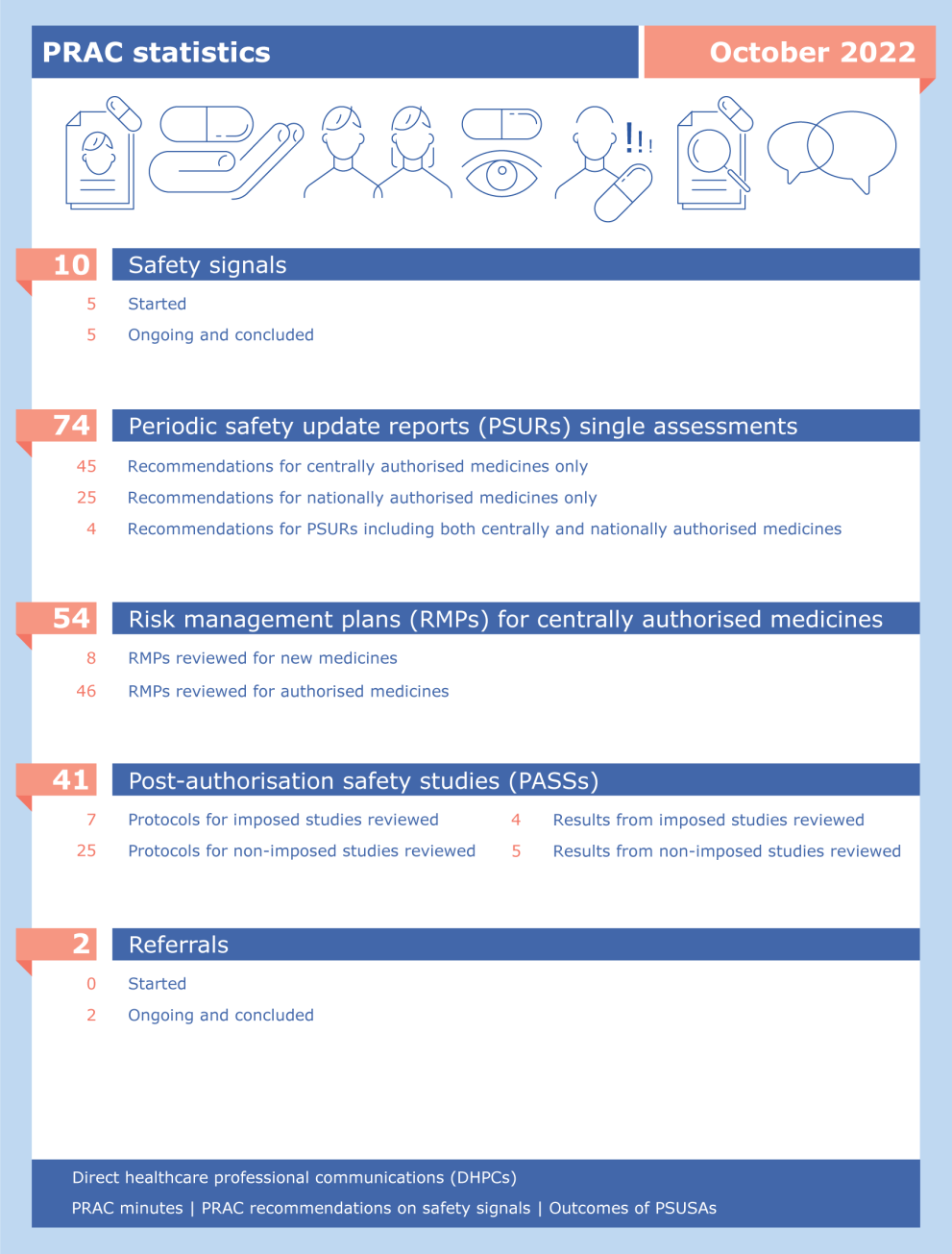
PRAC statistics: October 2022
Glossary:
- Safety signal assessments. A safety signal is information which suggests a new potentially causal association, or a new aspect of a known association between a medicine and an adverse event that warrants further investigation. Safety signals are generated from several sources such as spontaneous reports, clinical studies and the scientific literature. More information can be found under 'Signal management'.
- Periodic safety update reports, abbreviated as PSURs, are reports prepared by the marketing authorisation holder to describe the worldwide safety experience with a medicine in a defined period after its authorisation. PSURs for medicinal products that contain the same active substance or the same combination of active substances but have different marketing authorisations and are authorised in different EU Member States, are jointly assessed in a single assessment procedure. More information can be found under 'Periodic safety update reports: questions and answers'.
- Risk management plans, abbreviated as RMPs, are detailed descriptions of the activities and interventions designed to identify, characterise, prevent or minimise risks relating to medicines. Companies are required to submit an RMP to EMA when applying for a marketing authorisation. RMPs are continually updated throughout the lifetime of the medicine as new information becomes available. More information is available under 'Risk-management plans'.
- Post-authorisation safety studies, abbreviated as PASSs, are studies carried out after a medicine has been authorised to obtain further information on its safety, or to measure the effectiveness of risk-management measures. The PRAC assesses the protocols (aspects related to the organisation of a study) and the results of PASSs. More information can be found under 'Post-authorisation safety studies'.
- Referrals are procedures used to resolve issues such as concerns over the safety or benefit-risk balance of a medicine or a class of medicines. In a referral related to safety of medicines, the PRAC is requested by a Member State or the European Commission to conduct a scientific assessment of a particular medicine or class of medicines on behalf of the EU. More information can be found under referral procedures.
- Summary safety reports have been introduced as part of the enhanced safety monitoring of COVID-19 vaccines. Marketing authorisation holders are required to submit these reports to EMA, starting on a monthly basis. Their submission complements the submission of PSURs. For more information see Pharmacovigilance plan of the EU Regulatory Network for COVID-19 vaccines.
Ongoing referrals
Procedure | Status | Update |
|---|---|---|
| Janus Kinase inhibitors (JAKi) – Article 20 Referral | Under evaluation | PRAC continued its assessment |
| Amfepramone-containing medicinal products | Under re-evaluation | PRAC started re-examination |